Welcome to part 2 of our review of gastroenterology. Today we cover the various investigations commonly used to visualize the gastrointestinal tract and differential diagnoses of common complaints. As always, today's blog post is available in podcast form; look for "Med On The Go" on Podbean, iTunes, and Google Play.
Before we get into today's topic, first, a little reminder from last week's post:
What you should think of straight away when you see the
following phrases?
“Gum to bum” à
Crohn’s disease! It can affect any part/entire length of GI tract.
“Destruction to villi” à
coeliac disease! Also think about subsequent malabsorption symptoms such as
oily diarrhea and skin manifestations such as dermatitis herpetiformis
(vesicles filled with yellow fluid).
“Antibiotic use” à
C. difficile diarrhea!
“Megaloblastic anemia” à
ileum problem! Ileum is the site of B12 absorption!
Retroperitoneal structures (remember SAD PUCKER)
Suprarenal (adrenal) glands
Aorta/IVC
Duodenum (second to fourth segments)
Pancreas (tail is intraperitoneal)
Ureters
Colon (only the ascending and descending branches)
Kidneys
Esophagus
Rectum
Imaging
Esophagus, Stomach, and duodenum
·
Endoscopy
o
Best visualization of mucosa
o
Allows therapeutic intervention
§
Banding varices
§
Thermal therapy/clipping/injecting bleeding
ulcers
§
Dilatation treatment for esophageal strictures
·
Barium swallow
o
Can be considered if patient has dysphagia,
decreased level of consciousness (increases risk of aspiration), inability to
cooperate (increases risk of pharyngeal trauma), or possibility of fistulas
Jejunum and ileum
·
Barium small bowel follow through—low sensitivity
·
CT enterography—more accurate than barium small
bowel follow through but also low sensitivity.
·
MRI small bowel increasingly available
o
MRI enteroclysis—luminal contrast administered
by nasojejunal tube to dilate the small bowels—may improve sensitivity
·
“Double balloon” enteroscopy—enteroscope with
proximal and distal balloons to propel endoscope forward
o
Most sensitive
o
Only available in few institutions
o
Technically demanding
·
Wireless endoscopy capsule—small capsule is
swallowed and transmits images to a computer
o
Contraindicated in bowel obstruction
o
Can provide accurate diagnosis but no
intervention
Terminal ileum and colon
·
Colonoscopy +/- biopsy
o
Most common
o
Contraindicated if there is risk of perforation,
such as flare ups of acute diverticulitis or severe colitis
·
CT colonography
o
More accurate in diagnosing diverticulosis,
fistulae, and objects pressing down on the colon (e.g. ovarian cancer
compressing sigmoid colon).
o
Increasing evidence for use in screening,
especially to assess right side of colon (where colonoscopy is less sensitive).
o
More often used when optical endoscopic
colonoscopy is a risk (e.g. frail elderly) or unsuccessful (e.g. stricture).
Biliary or pancreatic duct
·
ERCP
o
Good for imaging and high probability for
intervention or biopsy of tissue sample
·
MRCP
o
As accurate as ERCP in determining bile duct
obstruction but less accurate in determining the cause of the obstruction
Important reminders:
1.
Epigastic pain—remember to rule out myocardial
infarction, dissecting aneurysm, pneumonia, or other thoracic sources of pain.
2.
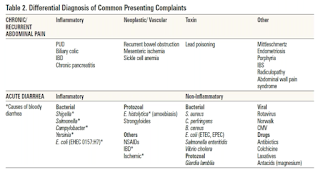
Inflammatory diarrhea—will have systemic
symptoms and BLOOD! Non-inflammatory diarrhea will NOT have systemic symptoms.
3.
Obscure but treatable causes of abdominal pain:
a.
Acute intermittent porphyria
b.
Hereditary angioedema
c.
Familial Mediterranean fever
d.
Vasculitis (e.g. polyarteritis nodosa)
a.
CNS disease
b.
Drugs
c.
Uremia
d.
Marijuana (cannabinoid hyperemesis)
e.
Pregnancy
2 The 6 big fat Fs!
a.
Fat
b.
Feces
c.
Flatus
d.
Fetus
e.
Fluid
f.
Fatal growth
1 Bowel ischemia
a.
Occurs most often at watershed areas, such as
splenic flexure and rectosigmoid junction
b.
Acute onset crampy left abdominal pain but
absence of abdominal tenderness on exam, rectal bleeding
c.
Patient is at risk of embolization,
atherosclerosis, and atrial fibrillation