As usual, today's post is available in podcast form; look for Med On The Go on iTunes, Google Play, and Podbean www.medonthego.podbean.com. Subscribe so you'll never miss an episode! Also be sure to visit our Facebook page www.facebook.com/drolimedonthego/ for updates and light-hearted mini-posts. If you enjoy our podcast and free notes, please also consider becoming a patron of the show! Visit www.patron.podbean.com/medonthego for more information.
Now, onto today's topic:
Now, onto today's topic:
Trauma is the leading cause of death in patients under 45
years old. It causes more deaths in children/adolescents than all diseases
combine. Trauma leads to a trimodal distribution of death: within minutes
(lethal injuries such as severe damage to the cardiac box—sternal notch,
nipples, and xiphoid process—or torn aorta which usually causes death at the
scene), within “golden hour” 4~6 hours (decreased mortality with trauma care),
and within days to weeks due to conditions such as multiple organ failure or
sepsis. Injuries can be separated into two categories: blunt (most common—motor
vehicle collisions, falls, assaults, sports) and penetrating (increasing in
incidence—gunshot wounds, stabbing, impalement).
High-risk injuries:
·
Motor vehicle collisions at high speed,
resulting in ejection from the vehicle
·
Motorcycle collisions
·
Vehicle vs. pedestrian crashes
o
Waddle’s triad:
§
Tibia-fibula or femur fracture
§
Truncal injury
§
Craniofacial injury
·
Fall from height > 12ft (3.6m, roughly 1
storey)
60% of MVC-related deaths are due to head injuries.
Head Injuries
·
Fractures—diagnosis with non-contrast CT and
physical exam
o
Skull fractures
§
Vault fractures
·
Linear, non-depressed
o
Most common
o
Typically occurs over temporal bone, in area of
middle meningeal artery (commonest cause of epidural hematoma)
o
Depressed—open (associated overlying scalp
laceration and torn dura, skull fracture disrupting paranasal sinuses or middle
ear) vs. closed
§
Basal skull
·
Typically occur through the floor anterior
cranial fossa (longitudinal more common than transverse)
·
Clinically diagnosis easier than imaging on CT
·
Battle’s sign—bruised mastoid process
·
Haemotympanum
·
“Raccoon eyes” periorbital bruising
·
CSF rhinorrhea/otorrhea
o
Facial fractures
§
Neuronal injury
§
Beware of open fractures or sinus fractures
(risk of infection)
§
Severe facial fractures may lead to airway
compromise due to profuse bleeding—secure airway is first priority!
·
Scalp Lacerations
o
Can be a source of significant bleeding
o
Achieve hemostasis, then inspect and palpate
skull for skull bone defects and order CT head to rule out skull fractures
·
Neuronal injuries
o
Diffuse
§
Mild traumatic brain injury (TBI) = concussion
·
Transient alteration in mental status that may
involve loss of consciousness
·
Hallmarks of concussion: confusion and amnesia,
which may occur immediately or within several minutes after injury
·
Loss of consciousness duration must be less than
30min; initial GCS must be 13~15, and post-traumatic amnesia must last less
than 24hrs
§
Diffuse axonal injury
·
Mild: coma 6~24 hours, with possible lasting
deficits
·
Moderate: coma > 24 hours, with little or no
brainstem dysfunction
·
Severe: coma > 24 hours, with frequent signs
of brainstem dysfunction
o
Focal
§
Contusions
§
Intracranial hemorrhage (epidural, subdural, or
intracerebral)
Warning signs of severe head injury:
·
GSC < 8
·
Deteriorating GCS
·
Unequal pupils
·
Lateralizing signs
Remember: altered level of consciousness is a hallmark of
brain injury!
History:
·
Pre-hospital status
·
Mechanism of injury
Physical Examination:
·
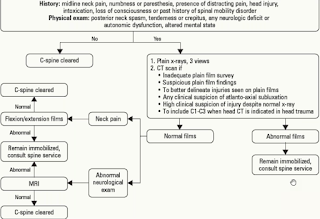
Assume C-spine injury until ruled out
·
Vital signs
o
Is there shock? Not likely caused by isolated
brain injury, except infants. Need to look for other conditions if shock is
present.
o
Is there increased intracranial pressure? Check
for Cushing’s response of irregular respirations, bradycardia, and
hypertension.
·
Severity of injury, as indicated by:
o
Level of consciousness
§
Mild—GCS 13~15; moderate—9~12; severe—3~8
§
“GCS 8, intubate”
§
Any change in GCS score of 3 or more indicates
serious injury
o
Pupils
§
Size
§
Anisocoria (difference in pupil size) > 1mm
in patient with altered LOC
§
Response to light
o
Lateralizing signs (motor/sensory) may become
more subtle with increasing severity of injury
Investigation
·
Laboratory: CBC, electrolytes, INR/PTT, glucose,
toxicology screen
·
Imaging
o
Non-contrast CT head
o
C-spine
o
Canadian CT Head Rule: CT Head is only required
for patients with minor head injury (witnessed loss of consciousness, definite
amnesia or witnessed disorientation in a patient with GCS 13~15) with any one
of the following:
§ GCS score < 15 at 2 hr. after
injury
§ Suspected open or depressed skull
fracture
§ Any sign of basal fracture
§ Vomiting > 2 episodes
§ Age > 65
§ Amnesia before impact > 30
min (cannot recall events just before impact).
§ Dangerous mechanism (e.g. pedestrian
struck by motor vehicle, occupant ejected from motor vehicle, or fall from
height > 3ft or 5 stairs.)
*Red indicates high risk factors (for neurological
intervention), and yellow
indicates medium risk factors (brain injury will show up on CT).
*Rule does not apply for
non-trauma cases, GCS < 13, age < 16, for patients on Coumadin and/or
having a bleeding disorder, or having an obvious open skull fracture.
Management
·
Goal in ED: reduce secondary injury by avoiding
hypoxia, ischemia, decreased CPP, or seizure
·
General
o
DRABC
o
Ensure oxygen deliver to brain through
intubation and prevent hypercarbia
o
Maintain BP (systolic > 90)
o
Treat other injuries—prioritize most
life-threatening injuries first while maintaining cerebral perfusion.
·
Early neurosurgical consultation for acute and
subsequent patient management
o
Seizure treatment/prophylaxis
§
Benzodiazepines, phenytoin, phenobarbital
§
Steroids are of no proven value
o
Treat suspected raise ICP:
§
Intubate
§
Sedate if risk for high airway pressures or
agitation
§
Hyperventilate (with 100% O2) to a pCO2 of 30~35
mmHg
§
Elevate head of bed to 20 degrees
§
Maintain adequate BP to ensure good cerebral
perfusion
§
Give mannitol 1g/Kg infused rapidly
(contraindicated in shock or renal failure)
·
Neurosurgical ICU admission for severe head
injuries
·
For minor head injuries (see definition above),
provide 24h head injury protocol to competent caregiver, follow up with
neurology as seemingly minor head injury can cause lasting deficits.
Mild Traumatic Brain Injury
·
75% of traumatic brain injuries are mild; the
rest are moderate or severe.
·
Highest rates in children 0~4yrs, adolescents
15~19yrs, and elderly > 65.
·
Clinical presentations
o
Somatic: headache, sleep disturbance, nausea and
vomiting, blurred vision
o
Cognitive: attention impairment, slower
processing speed, drowsiness, amnesia (REMEMBER: EXTENT OF RETROGRAD AMNESIA
CORRELATES WITH SEVERITY OF INJURY)
o
Emotional and behavioral: depression,
irritability, impulsive behavior
o
Severe concussion: may precipitate seizure,
bradycardia, hypotension, sluggish pupils
·
Etiology
o
Anything from falls and sports to MVC and
assault
·
Investigation
o
Neurological exam
o
Concussion recognition tool
o
Non-contrast CT head as per Canadian CT head
rules
o
MRI if symptoms worsen despite normal CT
·
Treatment
o
Close observations (especially for intracranial
complications)
o
C-spine collar until clearance* with lateral
C-spine X-ray (95% of radiologically visible abnormalities are found on this
film—so it’s the most important investigation!)
o
Admit if abnormal CT, GCS < 15, seizures, or
bleeding diathesis
o
Discharge only after normal CT with no other
complications; instruct to return to ED if clinical features develop/change
o
Appropriate follow up
o
Early rehabilitation to maximize outcome
o
Pharmacological management of pain, headache,
depression
o
Follow Return To Play guidelines
·
Prognosis
o
Most recover with minimal treatment
o
Athletes with previous concussions are at risk
of cumulative brain injury
o
Repetitive traumatic brain injuries can lead to
life-threatening cerebral edema and/or permanent impairment
*Every patient with one or more of the following symptoms or
signs should be placed in a C-spine collar:
·
Midline tenderness
·
Neurological symptoms or signs
·
Significant distracting injuries
·
Head injuries
·
Intoxication
·
Dangerous mechanism
·
History of altered level of consciousness