As usual, the following post is available in podcast form at www.medonthego.podbean.com. Feel free to also check out our Facebook page at www.facebook.com/drolimedonthego/. If you enjoy and wish to support our work please visit www.patron.podbean.com/medonthego for more details.
By definition, peptic ulcer disease refers to focal defects
in the mucosa of the stomach and duodenum that penetrate the muscularis mucosal
layer, resulting in scarring (defects superficial to the muscularis mucosa are
erosions and do not cause scarring.
(Quick review of anatomy: the GIT contains four layers. The
inner most layer is the mucosa—which includes epithelium, lamina propria, and
muscularis mucosa—followed the sub mucosa, muscularis propria, and adventitia.
Helicobacter
pylori, previously Campylobacter
pylori, is a gram-negative, microaerophilic bacterium found usually in the stomach. It was identified in 1982 by
Australian scientists Barry
Marshall and Robin
Warren, who found that
it was present in a person with chronic gastritis and gastric
ulcers, conditions not
previously believed to have a microbial cause. It is also linked to the
development of duodenal ulcers and stomach cancer. More than 50% of the world's population harbor H. pylori in
their upper gastrointestinal tract, more common in developing countries. However, over 80% of
individuals infected with the bacterium are asymptomatic.)
Etiology
|
|
Duodenal
|
Gastric
|
|
H. Pylori
|
90%
|
60%
|
|
NSAID
|
7%
|
35%
|
|
Idiopathic
|
15%
|
10%
|
|
Physiologic (stress-induced)
|
<3%
|
<5%
|
|
Zollinger-Ellison Syndrome
|
<1%
|
<1%
|
(Another brief review: Zollinger-Ellison syndrome is a rare condition in which one
or more tumors form in your pancreas or the upper part of your small intestine
(duodenum). These tumors, called gastrinomas, secrete large amounts of the hormone
gastrin, which causes the stomach to produce too much acid.)
Ulcers not related to H. Pylori or NSAIDs are becoming more
commonly recognized; these include CMV, cirrhosis of the liver, COPD, chronic
renal failure, ischemic and idiopathic causes. Cigarette smoking has been
linked to peptic ulcer disease; smoking not only impairs healing but also increases
the risk of ulcers, complications, and death. In contrast to popular belief,
alcohol consumption damages the gastric mucosa but does not cause ulcers.
Clinical presentation
·
Dyspepsia
o
Most common presentation
o
Only 5% will have ulcers—most have functional
disease
o
Can present with complications
§
Bleeding—most common! 10% The bleeding can be severe
if from the gastroduodenal artery
§
Perforation (usually from anterior ulcers) 2%
§
Gastric outlet obstruction 2%
§
Posterior inflammation (penetration) 2% and can
cause pancreatitis
·
Duodenal ulcers
o
History alone is very similar to that of
functional dyspepsia
o
6 classical features
§
Epigastric pain: may localize to tip of xiphoid
§
Burning sensation
§
Develops 1~3 hours after meals
§
Relieved by eating and antacids
§
Interrupts sleep
§
Periodicity (tends to occur in clusters over a
week with subsequent periods of remission)
·
Gastric ulcers
o
More atypical symptoms
§
Dull aching pain, often right after eating.
§
Eating will not relieve pain!
§
Dyspepsia or acid reflux
§
Episodes of nausea
§
A noticeable loss of appetite
§
Unplanned weight loss
o
A BIOPSY REQUIRED to rule out malignancy (whereas
duodenal ulcers are rarely malignant.)
Investigations
·
Endoscopy (most accurate)
·
Upper GI series
·
H. Pylori tests
·
Fasting serum gastrin measurement if
Zollinger-Ellison syndrome suspected—but most common cause of elevated serum
gastrin level is atrophic gastritis.
Treatment
·
Specific management depends on etiology
·
Eradicate H pylori if it is present
·
Stop NSAIDs if possible
·
Start proton-pump inhibitors PPI
o
Inhibits parietal cell H+/K+-ATPase pump which
secretes acid
o
Will heal most ulcers even if NSAIDs are
continued
o
Other medications such as histamine
H2-antagonists are less effective
·
Stop smoking
·
No diet modification required but some people have
fewer symptoms if they avoid coffee, alcohol, and spices
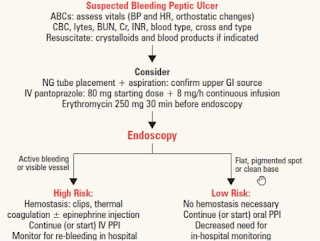
Management of bleeding peptic ulcers
·
Endoscopy (OGD) to explore upper GI tract
·
IV pantoprazole continuous drip
·
Evaluate risk of rebleeding/continuous bleeding
(most ulcers will stop bleeding spontaneously
o
Clinical risk factors: increased age (>60),
bleeding diathesis, history of peptic ulcer disease, comorbid disease,
hemodynamically unstable (transfusion required)
o
Endoscopic signs of recurrent bleeding are more
predictive than clinical risk factors: active bleeding, visible vessel, clots,
red spots
o
If high risk, consider ICU admission
H. Pylori-induced peptic ulceration
Pathophysiology
·
H. Pylori are Gram-negative flagellated rod that
resides within the gastric mucosa, causing persistent infection and
inflammation.
·
Acid secreted by parietal cells (stimulated by
vagal acetylcholine, gastrin, histamine) is necessary for most ulcers
·
No satisfactory theories of how H. pylori causes
ulcers, but pattern of colonization correlates with outcome
o
Gastritis only in antrum (15% of patients) and
high gastric acid are associated duodenal ulcer and may progress to gastric
metaplasia of duodenum where ulcer forms.
o
Gastritis through stomach (“pangastritis”—85% of
patients) and low gastric acid are associated with stomach ulcer and cancer.
Epidemiology
·
H. Pylori is found in about 20% of all Canadians
·
Highest prevalence in those raised during the
1930s
·
Infection most commonly acquired in childhood,
presumably by fecal-oral route
·
High prevalence in developing countries,
particularly in those of low socioeconomic status (poor sanitation and
overcrowding)
Outcome
·
Non-erosive gastritis in 100% of patients but asymptomatic
·
Peptic ulcer in 15% of patients
·
Gastric carcinoma and mucosal associated
lymphomatous tissue (MALT) lymphoma in 0.5% of patients
·
Most are asymptomatic but still worthwhile
eradicating to lower future risk of peptic ulcer/gastric malignancy and prevent
spread to others (mostly children <5 years)
Diagnosis
·
Non-invasive
o
Urea breath test
§
90~100% sensitivity
§
89~100% specificity
§
Can be falsely negative when on PPI therapy
o
Serology
§
88~99% sensitivity
§
89~95% specificity
§
Can remain positive after treatment
·
Invasive (requires endoscopy)
o
Histology
§
93~99% sensitivity
§
95~99% specificity
§
Gold standard!
§
Can be falsely negative when on PPI therapy
o
Rapid urease test (on biopsy)
§
89~98% sensitivity
§
93~100% specificity
§
Rapid
o
Microbiology culture
§
98% sensitivity
§
95~100% specificity
§
Research only
Treatment: H. Pylori eradication
·
Triple therapy for 7~14 days
o
PPI bid + amoxicillin 1g bid + clarithromycin
500mg bid
o
Becoming less successful as prevalence of H.
pylori clarithromycin-resistance on the rise
·
Quadruple therapy for 10~14 days now recommended
o
PPI bid + bismuth 525mg qid + tetracycline 500mg
qid +metronidazole 250mg qid
·
Levofloxacin can replace metronidazole or
tetracycline
·
Sequential therapy
o
5 days of PPI bid + amoxicillin 1g bid
o
6~10 days of PPI bid + clarithromycin 500mg bid,
tinidazole 500mg bid (generally substitute with metronidazole as tinidazole is
not available in Canada)
·
5~15% are resistant to all known therapies
NSAID-induced ulceration
NSAID use causes gastric mucosal petechiae in virtually all
erosions in most people and ulcers in some people (25%); erosions can bleed,
but usually only ulcers cause significant clinical problems. Most NSAID ulcers
are clinically silent—dyspepsia is as common in patients with ulcers as
patients without ulcers; NSAID-induced ulcers characteristically present with
complications such as bleeding, perforation, and obstruction. NSAIDs more
commonly cause gastric ulcers than duodenal ulcers. NSAID use may exacerbate
underlying duodenal ulcer disease.
Pathophysiology
·
Direct: erosions/petechiae are due to local
effect of drug on gastric mucosa
·
Indirect: systemic NSAID effect (intravenous
NSAID causes ulcers, but not erosions due to inhibition of mucosal
cyclooxygenase, leading to decreased synthesis of protective prostaglandins,
thus leading to ulcers
Risk factors for NSAID-induced peptic ulcer
·
Previous peptic ulcers or upper GI bleeding
·
Age >65
·
High dose of NSAID/multiple NSAIDs being taken
·
Concomitant corticosteroid use
·
Concomitant cardiovascular disease/other
significant disease
Management
·
Prophylactic cytoprotective therapy with PPI is
recommended if any of the above risk factors exist concomitantly with ASA/NSAID
use
·
Lower NSAID dose or stop all together and
replace with acetaminophen
·
Combine NSAID with PPI or misoprostol (less
effective) in one tablet
·
Enteric coating of aspirin provides minor
benefit since this decreases incidence of erosion, not incidence of ulceration
Stress-induced ulceration
Defined as ulceration or erosion in the upper GI tract of
ill patients, usually in ICU (the stress is physiologic not psychologic),
stress-induced lesions are most commonly in the fundus of the stomach. The
pathophysiology is unclear; it likely involves ischemia and may be cause by CNS
disease and acid hypersecretion.
Risk factors include:
·
Mechanical ventilation—most important
·
Anti-coagulation
·
Multi-organ failure
·
Septicemia
·
Severe surgery/trauma
·
CNS injury
·
Burns involving more than 35% of body surface
|
Curling’s ulcer
|
Cushing’s ulcer
|
|
Acute peptic ulcer of the duodenum resulting as a
complication from severe burns when reduced plasma volume leads to ischemia
and cell necrosis (sloughing) of the gastric mucosa.
Think: BURN from a CURLING iron!
|
Peptic ulcer produced by elevated intracranial pressure
(may be due to stimulation of vagal nuclei secondary to elevated ICP which
leads to increased secretion of gastric acid)
|
Clinical feature is painless upper GI bleeding. Treatment
includes prophylaxis with gastric acid suppressants to decrease the risk of
upper GI bleeding. PPI most potent but may increase risk of pneumonia; H2
blockers less potent but less likely to cause pneumonia. In active bleeding
ulcer the treatment is the same as covered above in peptic ulcer disease but
often less successful.