As always, this blog post is available in podcast form at www.medonthego.podbean.com. You can also find Med On The Go on iTunes and Google Play! For interest articles, useful quizzes, and funny medical jokes check out our Facebook page at www.facebook.com/drolimedonthego. If you wish to support us, please visit www.patron.podbean.com/medonthego for more details. Thanks!
75% of all gastrointestinal bleeds are classified as upper GI bleeds. An upper GI bleed is defined as a bleeding taking place proximal to the ligament of Treitz, a suspensory ligament where the fourth portion of the duodenum transitions to the jejunum.
75% of all gastrointestinal bleeds are classified as upper GI bleeds. An upper GI bleed is defined as a bleeding taking place proximal to the ligament of Treitz, a suspensory ligament where the fourth portion of the duodenum transitions to the jejunum.
Etiology
·
Above the GE junction
o
Epistaxis
o
Esophageal varices (10~30%)
o
Esophagitis
o
Esophageal cancer
o
Mallory-Weiss tear (10%)
·
Stomach
o
Gastric ulcer (20%)
o
Gastritis (20%)
o
Gastric cancer
o
Gastric antral vascular ectasia (rare condition
where small blood vessels are dilated around the antrum of the stomach—resulting
in “watermelon stomach”; associated with cirrhosis, chronic kidney failure, and
collagen vascular disease.)
o
Dieulafoy’s lesion (very rare where a large,
tortuous arteriole in the submucosa of the stomach erodes and bleeds)
·
Duodenum
o
Ulcer in bulb (25%)
o
Aortoenteric fistula: rare and lethal; usually
only if previous aortic graft has been done
·
Coagulopathy (drugs, renal disease, liver
disease)
·
Vascular malformation
Clinical features includes patient noticing blood is coming
out his/her GIT. This can be in a variety of forms. In order of decreasing
severity of the bleed: hematochezia (blood—usually fresh—passed through anus,
can be along with or mixed in stools), hematemesis (vomiting up blood—usually
fresh), coffee ground emesis (vomiting old blood), melena (old blood passed
through anus), and occult blood in stool.
ALWAYS ask about NSAID, aspirin, or anticoagulant drug use!
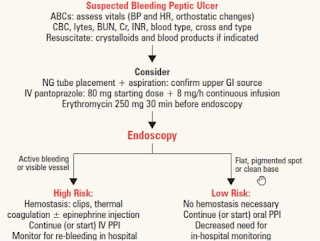
Initial management
1.
Resuscitate patient with 2 large bore IVs, IV
fluids, monitor vital signs
2.
Send blood for CBC, cross and type, platelets,
prothrombin time (PT), partial thromboplastin time (PTT), electrolytes, BUN,
creatinine, and liver function tests.
3.
Keep the patient fasting
4.
NGT can be considered to determine upper vs.
lower GIT bleeding
5.
Endoscopy is done to establish bleeding site and
treat lesion
·
For bleeding peptic ulcers, the most commonly
used method of controlling bleeding is injection of epinephrine around bleeding
point and thermal hemostasis via bipolar electrocoagulation or heater probe.
Less often thermal hemostasis may be used alone. Injection alone is not
recommended
·
Endoclips
·
Hemospray—mineral blend powder specifically used
for endoscopic hemostasis. It absorbs water to form a cohesive and adhesive
mechanic barrier around the bleeding site.
6.
Administer PPI (IV) to decrease the risk of
rebleeding if endoscopic predictors of rebleeding are seen
·
PPI is given to stable the clot, not to
accelerate ulcer healing
·
If given before endoscopy, it decreases need for
endoscopic therapeutic intervention
7.
For variceal bleeds, administer octreotide 50
micrograms loading dose followed by constant infusion of 50 micrograms/hour
8.
Consider IV erythromycin or metoclopramide to
accelerate gastric emptying prior to gastroscopy to remove clots from stomach.
Review—PT vs. PTT
Both PT and PTT are tests done to assess whether the patient
has a coagulation problem. PTT stands for partial thromboplastin time
(sometimes also called activated partial thromboplastin time APTT) and measures
the function of the intrinsic coagulation pathway; PT stands for prothrombin
time and measures the function of the extrinsic coagulation pathway. The way to
remember the difference is this: the 2 T are no longer together à they are “exes” à PT measures extrinsic
pathway. Why are they not together anymore? Because one of them got the “7 year
itch” à
PT/extrinsic pathways deals with factor VII while PTT deals with all other
factors.
Prognosis
·
80% stop spontaneously
·
Peptic ulcer rebleeding occurs in 25% of
patients. If there is no rebleeding, mortality is low 2%; however, it rises to
10% if rebleeding occurs.
·
Endoscopic predictors of rebleeding includes:
spurt or ooze, visible vessel, or fibrin clot
·
H2-antagonists have little impact on rebleeding
rates and need for surgery
·
Esophageal varices have a high rebleeding rate
(55%) and mortality (29%)
·
Patients can be sent home if:
o
They are clinically stable
o
Bleeding was minor
o
No comorbidities
o
Endoscopy shows clean ulcer with no predictors
of rebleeding