As usual, today's post is also available in podcast form. Look for "Med On The Go" on Podbean, iTunes, and Google Play. Subscribe so you'll never miss an episode! Also feel free to check out our Facebook page at www.facebook.com/drolimedonthego. If you enjoy my work, please consider supporting me--visit www.patron.podbean.com/medonthego for more details!
Onto today's topic:
While eating gluten-free can be just a lifestyle choice, for
those with coeliac disease it is not a choice but a necessity. Now, perhaps
with the combination of advanced medicine, wheat consumption, and migratory
patterns, the diagnosis and worldwide distribution of coeliac disease is on the
rise. So let’s get to know one of the most common genetic diseases: coeliac
disease.
Essentially coeliac disease is an abnormality of the small
intestine mucosa due to a reaction to gluten, a protein found in cereals. As
mentioned previously, it is a genetic disease; HLA-DQ2 (chromosome 6) is found
in 80~90% of patients compared with 20% in the general population. Coeliac
disease can also be associated with HLA-DQ8 (up to 40% of Caucasians carry the
HLA alleles but will never develop the disease.) When gluten is digested, it is
broken down into gliadin, which is the toxic factor to those with coeliac
disease—the body attacks the gliadin and in the process damages its own villi;
interestingly, unlike other autoimmune diseases, coeliac disease is the only
autoimmune disease in which the antigen is actually recognized. However, like
other autoimmune diseases, when you get one, you tend to get more than
one—coeliac disease is associated with other autoimmune diseases, especially
Sjogren’s disease and thyroid disease.
Once thought to be a disease only affecting Caucasians,
coeliac disease is now diagnosed worldwide. It is more commonly found in women.
Family histories reveal that 10~15% of first-degree relatives will also be
affected. Coeliac disease can present any time from infancy (when cereals
introduced—peak presentation) to the elderly; it can lay dormant until
triggered by certain events (immigration or sickness or other).
A classic presentation of coeliac disease would be the
combination of diarrhea, weight loss, anemia, symptoms of vitamin/mineral
deficiency, and failure to thrive in infants. More common current presentations
include bloating, gas, and iron deficiency. The symptoms improve when gluten is
eliminated from the diet and deteriorate when gluten is reintroduced. Because
the disease is usually more severe in the proximal bowel, iron, calcium, and
folic acid deficiency is more common (as these are absorbed proximally) than
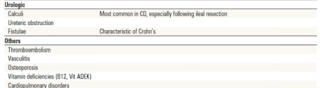
B12 deficiency (absorbed in ileum). Coeliac disease can be associated with
non-GIT conditions such as dermatitis herpetiformis skin eruptions (large
vesicles with yellow liquid), epilepsy, myopathy, depression, paranoia,
infertility, bone fractures, or metabolic bone disease.
The golden standard of diagnosis is small bowel mucosal
biopsy (usually from duodenum) showing increased intraepithelial lymphocytes
(earliest pathologic finding), crypt hyperplasia, and villous atrophy (which
can also be seen in small bowel overgrowth, Crohn’s disease, lymphoma, Giardia,
and HIV); however, serological tests can also be performed. Serum anti-tTG (tissue
transglutaminase) antibody, IgA, is 90~98% sensitive, 94~97% specific. IgA
deficient patients have false-negative anti-tTG; therefore, measure serum IgA
concomitantly via serum quantitative protein electrophoresis and incorporate
serum testing tTG and/or DGP (deamidated gliadin peptide) IgG in IgA
deficiencies. There will be evidence of malabsorption; these can be either
localized or generalized, such as steatorrhea, low levels of ferritin/iron
saturation, iron, calcium, albumin, cholesterol, carotene, and vitamin B12.
Consider CT enterography to visualize small bowel to rule out lymphoma.
Gluten-free diets should not be started before serological
tests and biopsy. Gluten is found in barley, rye, some oats, and wheat (mnemonic
BROW) and should be avoided in the patient’s diet; however, sometimes oats are
allowed if it is grown in soil without cross-contamination by other grains.
Rice and corn flour are acceptable. Supplementary of iron, folate, and other
vitamins/minerals should be added as necessary. If there is a poor response to
diet change, consider alternate diagnosis, concurrent disease (e.g. microscopic
colitis, pancreatic insufficiency), development of intestinal
(enteropathy-associated T-cell) lymphoma (symptoms include abdominal pain,
weight loss, and palpable mass), or development of diffuse intestinal
ulceration, characterized by aberrant intraepithelial T-cell population
(precursor to lymphoma).
Coeliac disease is associated with increased risk of
lymphoma, carcinoma (e.g. small bowel and colon; small increase compared with
general population), and autoimmune diseases. The risk of lymphoma may be
lowered by gluten-free diet.