This week we continue to explore inflammatory bowel disease:
Ulcerative colitis is defined as an inflammatory disease
affecting colonic mucosa anywhere from the rectum (ALWAYS involved) to the
cecum, causing anything from proctitis (rectum-only) to pancolitis (entire
colon); inflammation limited to rectum or left colon is more common than
pancolitis. On colonoscopy, the inflammation seen is diffuse, continuous, and
confined to the mucosa. The incidence of ulcerative colitis is 2~10/100,000 and
prevalence is 35~100/100,000. This makes it more common than Crohn’s disease.
Two-thirds of patients have disease onset by age 30, with a second peak after
age 50; like Crohn’s disease, the distribution is equal between male and female
patients. There is a small hereditary contribution—15% of cases have 1st
degree relative with disease. Risk is LESS in smokers.
The hallmark clinical feature of ulcerative colitis is
rectal bleeding. Diarrhea can also be present, as well as abdominal cramps/pain
(especially with defecation), tenesmus, urgency, and incontinence; systemic
symptoms include fever, anorexia, weight loss, and fatigue. The severity of the
colonic inflammation correlates with the symptoms (e.g. stool volume, amount of
blood in stool). Patients with ulcerative colitis present with characteristic
exacerbations and remissions; 5% of cases are fulminant.
Although there is no single confirmatory test, sigmoidoscopy
with mucosal biopsy is often sufficient for diagnosis, but a colonoscopy would
be helpful in determining the extent of disease (but contraindicated in severe
exacerbation). CT colonography (formerly barium enema) can be done if
colonoscopy not possible. Stool culture and microscopy and C. Difficile toxin
assay should be done to exclude infectious causes.
The mainstay of treatment is 5-ASA derivatives (suppository
and enema form in acute treatment; oral form can be used in maintaining
remission) and corticosteroids (IV for acute disease;
suppositories/enemas/topical applications can be used for disease distal to
splenic flexure) for mild to moderate disease; the use of 5-ASA medications
such as sulfasalazine or mesalamine may decrease rate of colorectal cancer. Immunosuppressants
(e.g. 6-MP) and biologics (e.g. infliximab) are used in hospitalized patients
with severe ulcerative colitis; biologics can also be used for outpatients with
moderate to severe disease, particularly those that are steroid-unresponsive or
steroid-dependent. Azathioprine can also be used in those who are
steroid-dependent, but they are most commonly used to maintain remission while
corticosteroids are being withdrawn; when given together with biologics,
azathioprine increases the efficacy of biologics and decreases the likelihood
of tolerance to biologics (around 10% chance/year). Diet change is of little
value in decreasing inflammation but may alleviate symptoms. Anti-diarrheal
medications are generally not used in ulcerative colitis. When all else fails, colectomy
is a curative option; bowel continuity can be restored with ileal pouch-anal
anastomosis (IPAA). Other indications of colectomy include toxic megacolon,
uncontrollable bleeding, pre-cancerous changes detected by
endoscopy/colonoscopy/biopsy, overt malignancy, or inability to taper
corticosteroids.
Complications of ulcerative colitis are similar to that of
Crohn’s disease, except that there are more liver problems involved in
ulcerative colitis (especially primary sclerosing cholangitis in men). There is
a greater risk of colorectal cancer in ulcerative colitis; the risk increases
with duration and extent of disease and also increases with active mucosal
inflammation and development of sclerosing cholangitis. Thusly, regular
colonoscopy and biopsy in pancolitis of ≥ 8 years is indicated. Toxic
megacolon (traverse colon diameter > 6cm on abdominal x-ray) with immediate
danger of perforation is also a major complication! This is lethal and requires
immediate treatment using steroids +/- surgery.
A comprehensive list of complications of ulcerative colitis
is as follows:
Urinary calculi
Liver problems
Cholelithiasis
Epithelial problems
Retardation of growth/sexual maturation
Arthralgia
Thrombophlebitis
Iatrogenic complications
Vitamin deficiencies
Eye problems
Colorectal cancer
Obstruction
Leakage (perforation)
Iron deficiency
Toxic megacolon
Inanition (wasting)
Strictures
In patients with only proctitis, the disease usually runs a
benign course. However, most patients present in chronic relapse pattern. More
colonic involvement in the first year of onset correlates with increased
severity of attacks and increased colectomy rate. Post colectomy most patients
can have normal life expectancy.
The biggest difference between Crohn’s disease and
ulcerative colitis is that Crohn’s disease can affect any part of the GIT where
as ulcerative colitis is limited to the large intestines.
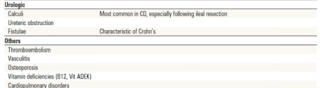
And as promised... the bonus chart of extra-intestinal manifestations of IBD!







No comments:
Post a Comment